
Becoming a parent is an amazing experience filled with many different emotions–joy, excitement, anticipation, fear, and worry to name a few. At least for me, there were constant questions swirling in my mind about how to best care for my little one. A lot of those questions were centered on how to feed my baby in a way that would help with optimal growth and development. Having a background in nutrition for infants and children has been extremely helpful for me, but I have still had questions come up time and again that I’ve wanted to look into to clarify my understanding and learn about on a deeper level. It’s a constant learning process!
So with this post, my goal is to help you understand how to feed your baby during the first two years of their life and feel confident in doing so. There are several feeding transitions during those first two years, so I hope having a lot of the information in one place will be helpful for you! We’ll touch on information regarding breastmilk and formula, when to start solid foods, how to start them, what to be mindful of when starting solids, when to offer water or cow’s milk, and a few other recommendations.
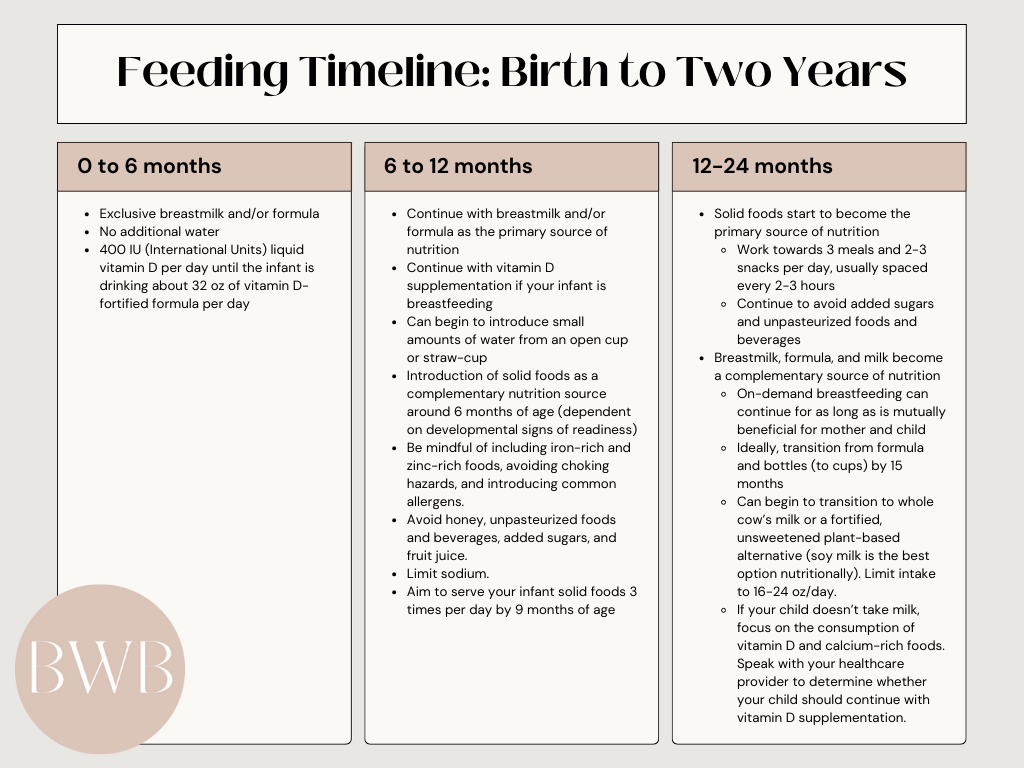
This is by no means an exhaustive list of all the information you will ever need to feed your baby (and I’ll provide more information on some topics in the future), but I also know it is a lot of information coming at you all at once. This is not meant to be overwhelming! Rather, I hope it will help you gain a big-picture view of the information and recommendations that are out there and help you feel like you are set up for success when it comes to feeding your baby. If it feels like information overload, take it a piece at a time and focus on where your baby is now! The information below will be divided by age, so it’s easy to find what’s most relevant to your child at this specific time. There's also a "cliff notes" version below for a quick and easy reference.
Lastly, I also want to note that these recommendations are generalized for the majority of infants and children. There are certain conditions or situations in which these recommendations may change, so please speak with your healthcare providers for more specific guidance for your child.
0-6 months
Breastmilk and/or formula
Your baby should be drinking either breastmilk or formula exclusively for the first six months. You do not need to provide your baby with water at this time as they receive adequate hydration through breastmilk or formula. Additional water will also take up space in their small tummies, limiting the amount of breastmilk or formula they can consume and putting them at risk for inadequate nutrition and electrolyte imbalance.
Vitamin D
While your baby is able to get adequate nutrition of most vitamins and minerals through breastfeeding and formula consumption, vitamin D is one nutrient where supplementation is usually recommended.
If you are breastfeeding, it is recommended to provide your baby with 400 IU (International Units) of liquid vitamin D daily.1 Another option is for the breastfeeding parent to take 4,000-6,400 IU of supplemental vitamin D each day, which would usually require additional supplementation outside of prenatal/postnatal multivitamins.2,3 Because this is high-dose supplementation, you should discuss the risks and benefits with your doctor before pursuing this option.
If your baby is receiving all formula, it is recommended to provide them with 400 IU of liquid vitamin D daily until he/she is consistently taking at least 32 oz of vitamin D-fortified formula each day.1
And lastly, if your baby is breastfeeding and receiving formula, it is recommended to provide him/her with 400 IU of liquid vitamin D daily.1
6-12 months
Breastmilk and/or formula
During this time, you should continue to feed your baby breastmilk and/or formula, which will continue to be the primary source of nutrition for your baby until he/she reaches 12 months of age.
Water
You can also begin to introduce water using an open cup or a cup with a straw (I like this one because it doubles as an open cup and straw cup in one and was designed by a pediatric feeding specialist). It is recommended that an infant not drink more than 4 to 8 oz of water per day at this age.4
Solid Foods
In addition to breastmilk and/or formula, you can introduce solid foods to your baby around 6 months of age as a complementary nutrition source. However, 6 months is not the requirement for starting solid foods, rather there are developmental signs of readiness that your child should be showing prior to starting solids. This may mean that your baby starts solids a little after 6 months, and that’s okay! You may have heard to introduce solids around 4 months of age, but this is an outdated recommendation. The American Academy of Pediatrics (AAP) and World Health Organization (WHO) recommend starting solids at about 6 months.5 Therefore, it is not recommended to start solids before 6 months of age, with the potential for one exception (more on this in the allergies section).
The following are the developmental signs your baby should be showing prior to starting solids6
- The ability to sit upright on the floor with minimal assistance
- The ability to hold up their head without assistance and control their head movements
- The ability to bring items in their hand to their mouth
- Having an interest in mealtime–they watch you eat and try to grab at your food

How you choose to introduce solids is up to you and what you feel most comfortable with, whether that be through spoon feeding with purees, Baby Led Weaning, or a combination of the two. (Weaning, in this case, is not referring to the process of stopping your baby from breastfeeding or drinking from a bottle. Weaning, in much of the world, is also defined as introducing solid foods). Encourage your baby to consume a variety of food from all food groups–this is a crucial time for them to experiment with different flavors and textures.
Spoon feeding, also known as traditional weaning, is different than Baby Led Weaning. Traditional weaning is when parents put smooth or pureed food on a spoon and feed it to their baby. Over time, there is a transition to feeding textures that are lumpier and eventually transitioning to the baby picking up foods to feed themselves.
Baby Led Weaning (BLW), on the other hand, is letting your baby self-feed from the beginning rather than parents feeding their baby with a spoon. This involves providing your baby with soft foods, usually in a strip or wedge shape, that they can pick up, hold, and feed themselves. In BLW, your baby is in charge of feeding himself/herself and how much he/she eats. If you are looking for more information on BLW, I highly recommend the Solid Starts website and app.
If you’re feeling hesitant about committing to one method, there is room for flexibility in how you introduce solids to your baby. What is most important is that you feel comfortable and confident in your choice! So, you can also choose to do a combination of spoon feeding and BLW if that feels best for you and your baby.
Iron and Zinc-Rich Foods
Before your baby is born, they build up a reserve of iron in their body that, with a combination of breastmilk or formula, is usually sufficient for about the first 6 months of life. Once they reach 6 months of age, this reserve begins to deplete and their iron needs also increase.7 Iron is necessary to make hemoglobin, a protein in red blood cells, which helps to transport oxygen through the blood to the rest of the body. When iron is deficient, red blood cells are unable to carry sufficient oxygen throughout the body. Therefore, it is important to include iron-rich foods as your baby starts solids.
There are two types of iron, heme iron, and non-heme iron. Heme iron is found in animal foods and is more readily absorbed by the body. Non-heme iron is found in plant foods and is not as readily absorbed. However, both are important to help your child meet their iron needs. You can also pair iron foods with foods rich in vitamin C because vitamin C helps our body absorb more iron.
Iron-rich foods include
- Meat, poultry, and fish
- Beans, peas, lentils, and edamame
- Fortified cereals and oatmeal
- Nut and seed butters
- Tofu
- Dark green leafy vegetables such as spinach or kale
There are certain situations where an iron supplement may be necessary, so talk with your baby’s doctor to determine if this is the case for your baby.
Zinc needs also increase around 6 months and are not sufficiently met through breastmilk alone.8 The zinc content of human milk is initially high and well absorbed, however, the concentration of zinc declines during the first 6 months. Therefore, it is necessary to ensure your infant is also getting zinc-rich foods, which support immune function and growth.8 The good news is that many of the iron-rich foods and zinc-rich foods overlap!
Zinc-rich foods include
- Meat
- Beans
- Fortified cereals
- Nut and seed butters
- Whole grains
- Dairy products
Choking Hazards
When starting solids, it is important to keep in mind what common choking hazards you should avoid feeding your baby. Choking-hazard foods are typically round, hard, sticky, and/or slippery. These types of foods can be choking hazards even up to 4 years of age. The foods that fall into these categories should either be avoided altogether or modified to make them soft (so that you can mash it easily between two fingers) or fine (grated into small shreds or ground) and no longer spherical in shape (cut into spears or strips, for example). Here are some examples of choking hazards:
Round foods
- Grapes
- Grape or cherry tomatoes
- Blueberries
- Cherries
- Hot dogs
- String cheese (when left whole or cut into rounds)
Hard foods
- Raw fruits and vegetables such as apples and carrots
- Nuts and seeds
- Chips
- Pretzels
- Popcorn
- Some crackers
- Hard candy
- Tough and large pieces of meat
- Ice
Sticky Foods
- Globs of nut butter
- Soft bread, muffins, or pancakes
- Chewy candy like taffy, gum, gummy bears
- Gummy vitamins
- Fruit snacks
- Dried fruit
- Marshmallows
Allergies
It is also recommended to introduce allergenic foods (in a safe, age-appropriate form) early and often. Previous recommendations advised delaying the introduction of allergenic foods to infants until 1, 2, or 3 years of age depending on the food, but recent studies and research have shown that the introduction of allergenic foods early and often reduces the risk of developing food allergies.9
The top common allergens are
- Milk
- Eggs
- Peanuts
- Tree Nuts
- Fish
- Shellfish
- Wheat
- Soy
- Sesame

Your baby may be at an increased risk for food allergies if they have severe eczema or an existing allergy.6 If you are concerned about your baby’s risk for food allergies, talk to your healthcare provider for individualized recommendations, which could include introducing some allergenic foods earlier than 6 months.
An allergic reaction may not occur on the first exposure to a food, and can actually occur several exposures later. If your baby has a severe allergic reaction, call 911 right away. While this is not an exhaustive list, signs of a severe allergy may include difficulty breathing, wheezing, widespread hives, swelling of the mouth, lips, tongue, or face, sudden lethargy, pale/bluish skin, or repetitive vomiting.
If you would like more information regarding allergic reactions and how to introduce allergens, I would recommend reading the linked posts.
A Few Other Recommendations
There are a few additional recommendations to keep in mind when introducing solids, some of which are in regard to an infant’s safety.
Honey should not be introduced before 1 year of age, including cooked honey, such as in bread or marinades.6 This is because of the risk of botulism, a toxin that can contaminate honey. Because infants’ immune systems are not yet fully developed, they are at higher risk of being harmed by botulism.
Infants should not receive raw eggs or meat, unpasteurized foods, or high-mercury fish (shark, swordfish, fresh tuna, king mackerel, tilefish, etc.).6 Infants are at higher risk to get sick from raw and unpasteurized foods because their immune systems are not yet fully developed. Mercury can negatively affect their developing brain and nervous system.
The AAP, AHA, USDA, and HHS recommend no added sugars for children under 2 years of age. Added sugars do not provide the nutrients that infants need during this critical period of growth and development and can easily displace the nutrients they could otherwise be consuming from more nutrient-dense foods.6 Every bite counts for our little ones! Added sugars can also lead to an increase in cavities and increase the risk for some types of disease. Taste preferences are also being formed during this time, and infants and children may develop stronger preferences for overly sweet foods and be less willing to accept other foods. Is it the end of the world if your baby has a few tastes of something with added sugar here and there? Of course not! If you want your baby to eat cake on their first birthday, by all means do so. But as a general rule, it is best to avoid offering added sugars and rather focus on providing young infants with more nutrient-dense foods as often as possible.
Fruit juice should not be introduced before 12 months.4,6
It is recommended that sodium be limited in an infant’s diet. Sodium plays an important role in the body, such as fluid regulation and neurologic function, but too much sodium can be harmful. Our babies do get some sodium from breastmilk and formula, and sodium naturally exists in some foods. Too much sodium/salt introduced early can lead to taste preferences for high-sodium foods and increase the risk for the development of some diseases later in life.6 A few simple ways to reduce your infant’s sodium intake include choosing fresh foods over processed foods, not adding salt to their food, and choosing low-sodium food options or rinsing their food underwater (for example, rinsing canned beans). A small amount of salt added to your family’s meal should be okay, but choose to season your baby’s plate with herbs and spices rather than salt.
Once your baby reaches 9 months, aim to provide him/her with an opportunity to eat solid foods 3 times each day. This helps to set them up for success when they transition to solid foods as the primary source of nutrition.
12-24 months
Once your child is 12 months old (now entering toddler territory!), solid foods are starting to become their primary source of nutrition. This is still somewhat of a transition period so not everything has to change immediately the moment they turn one. We are aiming to get to about three meals and two to three snacks each day, usually spaced two to three hours apart. However, for a little while some snacks may still be breastmilk or formula as you work through this transition. On-demand breastfeeding can continue well beyond the one-year mark, for as long as it is mutually beneficial for mother and child. But keep in mind that it is now becoming a complementary nutrition source rather than the primary nutrition source. Ideally, the goal is to wean from formula and all bottles (to cups) by 15 months.
At this point, you can begin to transition to plain, pasteurized, whole milk or an unsweetened milk alternative (more on this in a minute!). Milk and milk alternatives should not be introduced as a beverage before 12 months because they do not have the necessary nutrients that infants need during that stage of development (it is okay to cook with it!).4,6 It is also more difficult for infants’ digestive systems and kidneys to process the higher protein and mineral content found in cow’s milk before 12 months. Whole milk is recommended for children under 2 years as they still need the higher fat content to support normal growth and brain development. The fortification of vitamin D and calcium is also important for a child’s nutrition. Milk intake should be limited to about 16-24 oz per day per AAP recommendations. The reason for this is to ensure that milk is not displacing the nutrition that toddlers need from solid foods by decreasing their appetite. For cow’s milk specifically, too much can also result in constipation and put your child at higher risk for developing anemia.
Not all plant-based milk is created equal, so it is important to look for options that are unsweetened, fortified with vitamin D and calcium, and have similar nutrition content to cow’s milk (particularly calories and protein). Currently, fortified soy milk is the only plant-based alternative that is considered to be a dairy equivalent, and is the best option for a plant-based alternative.6,10 However, soy may not be the best option for all children (particularly those with a soy allergy or sensitivity), so a fortified pea protein or oat milk beverage would be the next best option, combined with a varied and well-balanced diet. If you are concerned with your child’s nutrition or growth, work with your healthcare providers to determine the best options for your child.
If your child refuses to take milk altogether, all is not lost! They can still get adequate nutrition from consuming a variety of other foods. Vitamin D and calcium are the main nutrients that milk provides, but you can find calcium in other dairy products, such as yogurt and cheese, and in almonds, dark leafy greens, and fortified soy products such as tofu (just remember to prepare these foods in a safe way to minimize choking hazards). There are fewer food options for vitamin D, but fatty fish, liver, egg yolks, and some mushrooms are the best sources. It is not uncommon for a child to continue on vitamin D supplementation, however, consult with your healthcare provider to determine how long supplementation is necessary for your child.
A quick note on toddler formulas/drinks–these are usually unnecessary and not recommended as a nutrition source for your child. They typically contain added sugars and other preservatives and are also expensive. There are some situations where a toddler formula or drink may be indicated (to help with weight gain for example), however, this should always be discussed with your healthcare providers.
While whole fruit is still preferred (thanks to the additional nutrients it provides, including fiber), 100% fruit juice can be introduced but should be limited to 4 oz per day. Continue to avoid juices and other drinks that contain added sugars. More sodium can be tolerated at this age compared to 6 months, but it is still helpful to limit excess sodium where possible.
Overall, aim to provide your child with a variety of textures and flavors and include foods from all food groups. Work with your healthcare providers to address any questions or concerns you may have with your child’s growth or eating abilities and to come up with a plan specifically tailored to your child and your family's circumstances.
Conclusion
Whew! We made it! I know learning about how to feed a baby over the first two years is a lot of information, but don’t worry about remembering everything right now. Save this post for later and come back when you have questions or need a refresher.
I hope that this post has been helpful for you, has given you confidence, and has taken out some of the guesswork in knowing how to go about feeding your children during the first two years of their lives. It is such a fun experience being able to watch your child grow in their ability to eat–from learning how to breastfeed or take a bottle, to seeing their reactions when trying foods for the first time, to seeing them eat with little spoons, to watching them figure out how to take bites and be able to move food around in their mouth to prepare for a swallow. It is a lot of hard work (for both the parent and the child) and takes a lot of patience on our end (cue the messes and food throwing!), but it really is a joyful and rewarding experience! Wishing you all the best with feeding your cute kiddos!
References
- Wagner CL, Greer FR, and the Section on Breastfeeding and Committee on Nutrition. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008;122(5):1142-1152. doi:10.1542/peds.2008-1862.
- Oberhelman SS, Meekins ME, Fischer PR, et al. Maternal vitamin D supplementation to improve the vitamin D status of breast-fed infants: a randomized controlled trial. Mayo Clin Proc. 2013;88(12):1378-1387. doi:10.1016/j.mayocp.2013.09.012
- Hollis BW, Wagner CL, Howard CR, et al. Maternal Versus Infant Vitamin D Supplementation During Lactation: A Randomized Controlled Trial [published correction appears in Pediatrics. 2019 Jul;144(1):]. Pediatrics. 2015;136(4):625-634. doi:10.1542/peds.2015-1669
- American Academy of Pediatric Dentistry. Healthy beverage consumption in early childhood: Recommendations from key national health and nutrition organizations: Summary of oral health considerations. The Reference Manual of Pediatric Dentistry. 2021:565-8.
- Meek JY, Noble L, Section on Breastfeeding. Policy statement: Breastfeeding and the use of human milk. Pediatrics. 2022;150(1). doi:10.1542/peds.2022-057988
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. 9th Edition. December 2020. Available at DietaryGuidelines.gov.
- Office of dietary supplements - iron. NIH Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/Iron-HealthProfessional/. Accessed February 24, 2023.
- Stanford Medicine Children's Health. Stanford Medicine Children's Health - Lucile Packard Children's Hospital Stanford. https://www.stanfordchildrens.org/en/topic/default?id=zinc-19-Zinc. Accessed February 24, 2023.
- Greer FR, Sicherer SH, Burks AW, et al. The effects of early nutritional interventions on the development of atopic disease in infants and children: The role of maternal dietary restriction, breastfeeding, hydrolyzed formulas, and timing of introduction of Allergenic Complementary Foods. Pediatrics. 2019;143(4). doi:10.1542/peds.2019-0281
- Verduci E, D’Elios S, Cerrato L, et al. Cow’s milk substitutes for children: Nutritional aspects of milk from different mammalian species, special formula and plant-based beverages. Nutrients. 2019;11(8):1739. doi:10.3390/nu11081739
Please note that this website does not provide medical advice. Any content provided by Begin With Balance is for informational purposes only and is not to be used as a substitute for medical advice or as diagnostic or treatment information. The information that is provided by Begin With Balance is created for a generalized audience. We understand that you or your child may have individual needs that are not considered in the information we provide. Begin With Balance does not provide professional advice to any users or their families. If you choose to engage in the information provided on this website, you do so at your own risk. Begin With Balance is not responsible for any adverse event that may result from engaging with our content. By using this website, you accept the responsibility for your own health and your family’s health. Please seek the advice of your specific medical or healthcare professional with any questions you may have regarding your health or your family’s health.



Leave a Reply